The Surprising Benefits of Intermittent Fasting
Introduction In recent years, intermittent fasting has gained significant popularity as a powerful and flexible dietary strategy. It involves cycling between periods of eating and fasting, with various methods and schedules to choose from. While it may seem like a trendy fad, intermittent fasting is backed by scientific research and has been shown to offer a multitude of health benefits beyond just weight loss. In this blog post, we will explore the many advantages of intermittent fasting, highlighting its impact on not only your waistline but also your overall well-being. 1. Weight Loss and Fat Loss One of the most well-known benefits of intermittent fasting is its effectiveness in promoting weight loss. By restricting your eating window, you naturally consume fewer calories, leading to a caloric deficit. However, it’s not just about eating less; intermittent fasting can also increase your metabolic rate and improve fat burning. This results in reduced body fat and, in some cases, can help preserve lean muscle mass. 2. Improved Insulin Sensitivity Intermittent fasting has been shown to enhance insulin sensitivity, a crucial factor in preventing and managing type 2 diabetes. By allowing the body to better regulate blood sugar levels, this eating pattern can reduce the risk of insulin resistance and help maintain healthy glucose metabolism. 3. Heart Health Studies have suggested that intermittent fasting may contribute to better heart health by lowering risk factors such as high blood pressure, elevated cholesterol levels, and inflammation. This could lead to a decreased likelihood of developing heart disease and its associated complications. 4. Cellular Repair and Longevity Fasting periods encourage a process known as autophagy, in which the body cleans out damaged cells and regenerates new ones. This cellular repair can help protect against various diseases and promote longevity. Some animal studies even suggest that intermittent fasting might extend lifespan, although more research is needed to confirm this in humans. 5. Enhanced Brain Function Intermittent fasting has a positive impact on brain health and cognitive function. It may improve brain-derived neurotrophic factor (BDNF), a protein associated with the growth and protection of brain cells. This can lead to enhanced memory, mood, and overall mental well-being. Some studies also suggest that intermittent fasting could potentially reduce the risk of neurodegenerative diseases like Alzheimer’s and Parkinson’s. 6. Reduced Inflammation Chronic inflammation is a contributing factor to numerous health issues, including autoimmune diseases and cancer. Intermittent fasting may help reduce inflammation by decreasing the production of pro-inflammatory markers. This can lead to a lower risk of inflammatory conditions and an overall improvement in immune function. 7. Enhanced Weight Management While intermittent fasting can promote weight loss, it can also help individuals maintain a healthy weight more easily. The flexibility of this eating pattern allows for greater control over calorie intake, making it easier to regulate your weight over the long term. 8. Simplicity and Flexibility Intermittent fasting is relatively easy to implement, making it a practical dietary strategy for many individuals. It doesn’t require complicated meal plans, special foods, or expensive supplements. Furthermore, there are various approaches to choose from, such as the 16/8 method, 5:2 diet, or alternate-day fasting, allowing you to tailor your fasting schedule to your preferences and lifestyle. Conclusion Intermittent fasting isn’t just another dieting trend; it’s a well-researched and evidence-based approach to improving your overall health and well-being. From weight loss and fat loss to better insulin sensitivity, heart health, and brain function, the benefits of intermittent fasting are diverse and compelling. If you’re considering trying it, consult with a healthcare professional to determine the best fasting approach for your individual needs. With its simplicity and numerous potential advantages, intermittent fasting may be the lifestyle change you’ve been looking for to enhance your health and quality of life.
The Role of Laser Surgery in Proctology
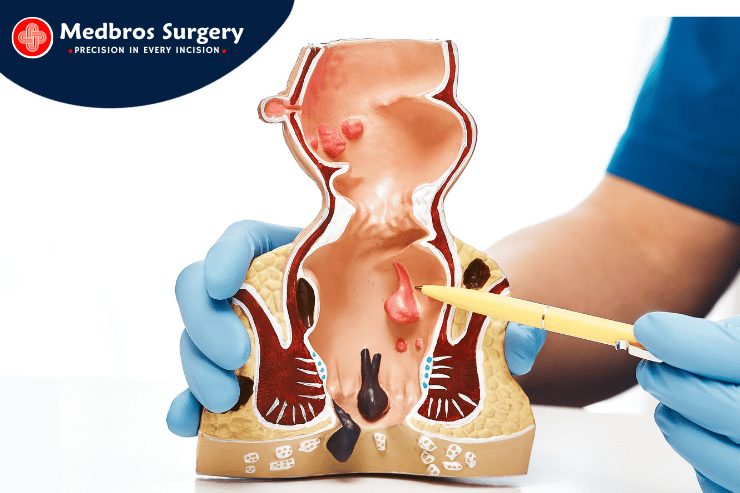
The Role of Laser Surgery in Proctology Introduction: Proctology, a branch of medicine that deals with the diagnosis and treatment of disorders related to the rectum and anus, has witnessed a significant transformation in recent years with the integration of laser surgery. This groundbreaking approach is changing the way proctologists diagnose and treat various conditions, offering patients a minimally invasive, less painful, and highly effective alternative to traditional surgical methods. In this blog post, we’ll explore the role of laser surgery in proctology and how it is revolutionizing the field. The Basics of Laser Surgery in Proctology: Laser surgery in proctology involves the use of highly focused beams of light (laser) to cut, vaporize, or remove tissues with remarkable precision. This technique is gaining popularity in proctology for its ability to treat various conditions, including hemorrhoids, anal fissures, and rectal tumors. 1. Hemorrhoid Treatment: Hemorrhoids, a common and often painful condition, can be effectively treated with laser surgery. Laser energy is used to shrink and destroy the hemorrhoidal tissue, providing relief from discomfort, bleeding, and swelling. The procedure is minimally invasive, resulting in less pain and faster recovery times compared to traditional surgical methods. 2. Anal Fissure Repair: Anal fissures, small tears in the anal lining, can cause excruciating pain and discomfort. Laser surgery can precisely target and repair these fissures, promoting faster healing and reducing the risk of recurrence. 3. Fistula and Abscess Management: Laser surgery has proven invaluable in treating anal fistulas and abscesses. The controlled application of laser energy allows for precise incision and drainage, reducing the risk of complications and promoting quicker healing. 4. Management of Rectal Tumors: Laser surgery has also found utility in the treatment of benign and early-stage malignant rectal tumors. Its precision allows surgeons to selectively remove tumor tissue while preserving healthy surrounding tissue, thus minimizing the risk of complications. 5. Polyp and Lesion Removal: In cases of benign polyps or lesions in the rectal or anal area, laser surgery provides a precise and effective method for removal. The focused energy of the laser minimizes damage to surrounding tissue, enhancing patient outcomes. Advantages of Laser Surgery in Proctology: The adoption of laser surgery in proctology comes with a range of benefits for both patients and healthcare providers: 1. Minimally Invasive: Laser surgery requires smaller incisions, leading to reduced post-operative pain, shorter hospital stays, and quicker recovery times. 2. Reduced Bleeding: The laser’s precision cauterizes blood vessels during surgery, minimizing bleeding during and after the procedure. 3. Lower Risk of Infection: Smaller incisions and reduced tissue trauma translate into a reduced risk of infection and complications. 4. Enhanced Precision: The focused nature of laser energy enables proctologists to precisely target problem areas, preserving healthy tissue. 5. Less Scarring: Smaller incisions result in minimal scarring, leading to better cosmetic outcomes. Future of Laser Surgery in Proctology: As technology continues to advance, the role of laser surgery in proctology is poised to expand further. Future trends may include: Robotic-Assisted Laser Surgery: Combining laser technology with robotic precision could enhance the accuracy and outcomes of proctological procedures. Minimally Invasive Colorectal Surgery: Laser surgery may play a more significant role in the treatment of colorectal diseases and conditions, offering patients an alternative to open surgery. Conclusion: Laser surgery in proctology represents a significant leap forward in the treatment of rectal and anal disorders. Its minimally invasive nature, precision, and reduced recovery times are transforming the way proctologists approach patient care. As technology continues to evolve, we can anticipate even more remarkable innovations in laser surgery, further improving the lives of patients facing proctological conditions. This evolving field underscores the bright future of proctology and the promise of better patient outcomes.
Advancements in Minimally Invasive Surgery
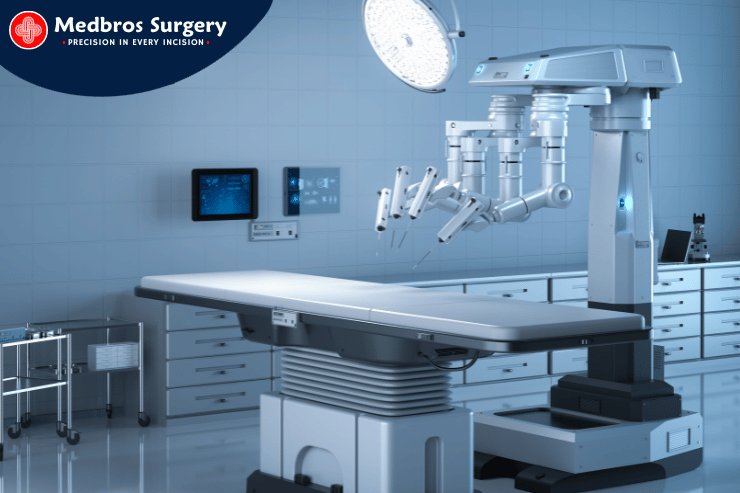
Advancements in Minimally Invasive Surgery: Pioneering Techniques Transforming Healthcare Introduction: In recent years, the field of surgery has witnessed a revolutionary transformation with the advent of minimally invasive techniques. These groundbreaking procedures have redefined surgical practices, offering patients safer and more efficient alternatives to traditional open surgeries. In this blog post, we’ll delve into the world of minimally invasive surgery, exploring the latest advancements that are reshaping the landscape of healthcare. The Evolution of Minimally Invasive Surgery: Traditionally, surgery often entailed large incisions, extended hospital stays, and prolonged recovery periods. However, with the introduction of minimally invasive techniques, surgeons can now perform complex procedures through small incisions, utilizing specialized instruments and advanced imaging technologies. 1. Laparoscopy: Laparoscopy, one of the pioneering techniques in minimally invasive surgery, involves the use of a thin, flexible tube equipped with a camera and surgical instruments. This approach provides surgeons with a clear, high-definition view of the surgical site, allowing for precise and controlled movements. 2. Robotic-Assisted Surgery: The integration of robotics into surgical procedures has ushered in a new era of precision and dexterity. Surgeons can now perform intricate surgeries with enhanced accuracy, thanks to robotic arms controlled by skilled surgeons. This technology offers 3D visualization, allowing for meticulous and delicate maneuvers. 3. Endoscopy: Endoscopic procedures involve the insertion of a thin tube with a camera and light source through natural body openings or small incisions. This technique is commonly used for procedures in the gastrointestinal tract, respiratory system, and other internal organs. Advantages of Minimally Invasive Surgery: The benefits of minimally invasive surgery extend beyond the operating room, profoundly impacting patients’ overall experience: 1. Faster Recovery Times: Minimally invasive techniques typically result in shorter hospital stays and quicker recovery periods. Patients can return to their daily activities sooner, minimizing disruption to their lives. 2. Reduced Pain and Discomfort: With smaller incisions and less tissue disruption, patients experience less post-operative pain and discomfort compared to traditional open surgeries. 3. Lower Risk of Complications: Minimally invasive procedures are associated with a lower risk of complications, such as infection and excessive bleeding, leading to improved patient safety. 4. Minimal Scarring: The smaller incisions in minimally invasive surgery often result in less noticeable scars, contributing to improved cosmetic outcomes. Future Trends in Minimally Invasive Surgery: As technology continues to advance, the future of minimally invasive surgery holds even more promise. Emerging innovations may include: – Augmented Reality (AR) and Virtual Reality (VR): These technologies offer surgeons immersive visualization and simulation, enhancing surgical planning and precision. – Natural Orifice Transluminal Endoscopic Surgery (NOTES): NOTES involves accessing internal organs through natural body openings, further minimizing external incisions. Conclusion: The rapid progress in minimally invasive surgery represents a monumental leap forward in the field of healthcare. These cutting-edge techniques are revolutionizing surgical practices, offering patients safer, more efficient, and less invasive alternatives. As technology continues to advance, we can anticipate even more remarkable innovations that will shape the future of surgery, ultimately improving the lives of patients worldwide.
The Role of Nutrition in Surgical Recovery
The Role of Nutrition in Surgical Recovery – Surgery is a significant event in one’s life, and the journey to recovery after a surgical procedure can be just as crucial as the surgery itself. While post-operative care, medications, and follow-up appointments are essential components of healing, one aspect often underestimated is the role of nutrition in the recovery process. The foods you eat can significantly impact the speed and success of your recuperation. In this blog post, we’ll explore the critical role of nutrition in surgical recovery and provide valuable insights into making the right dietary choices to support your healing journey. Nourishing Your Body for Recovery – Proper nutrition is the foundation for healing and regaining strength after surgery. Here’s why it matters: 1. Supports Tissue Healing : Surgery often involves incisions and tissue damage. Adequate protein intake is crucial for repairing and rebuilding damaged tissues. Lean protein sources like chicken, fish, beans, and tofu should be part of your post-surgery diet. 2. Enhances Immune Function : A well-balanced diet rich in vitamins and minerals, particularly vitamin C and zinc, can bolster your immune system. A strong immune system is essential for warding off infections and complications during the recovery period. 3. Reduces Inflammation : Omega-3 fatty acids found in fish, flaxseeds, and walnuts have anti-inflammatory properties. A diet high in these nutrients can help reduce post-surgical inflammation and discomfort. 4. Manages Constipation : Post-surgery pain medications can cause constipation. Consuming high-fiber foods such as fruits, vegetables, and whole grains can help regulate your digestive system and alleviate this common issue. 5. Maintains Energy Levels : Surgery can leave you feeling fatigued. Eating a well-balanced diet with complex carbohydrates (whole grains) can help maintain your energy levels and prevent weakness. 6. Promotes Wound Healing : Foods rich in vitamin A and vitamin K play a crucial role in the formation of new blood vessels and clotting. These vitamins can support the healing of surgical wounds. Post-Surgery Dietary Tips – To make the most of your nutrition during the recovery period, consider the following tips: 1. Stay Hydrated : Proper hydration is essential for recovery. Water helps your body process medications and flush out toxins. 2. Focus on Protein : Aim for lean proteins like chicken, fish, turkey, and plant-based sources like tofu and legumes. 3. Incorporate Fruits and Vegetables : These provide essential vitamins, minerals, and antioxidants that aid in the healing process. 4. Monitor Fiber Intake : Control constipation by including high-fiber foods in your diet. 5. Limit Sugary and Processed Foods : Excessive sugar and processed foods can hinder the healing process. Opt for whole, unprocessed foods. 6. Follow Your Surgeon’s Advice : Always follow the dietary recommendations provided by your surgeon or healthcare provider. They may have specific instructions tailored to your surgery and individual needs. Conclusion – Incorporating the right nutrition into your post-surgery recovery plan can make a substantial difference in the outcome. While every surgery is unique, a healthy and well-balanced diet is universally beneficial. Prioritize your recovery by paying attention to what you eat, and remember to consult your healthcare provider for personalized dietary guidance. By nourishing your body properly, you’ll increase your chances of a smoother, faster, and more successful surgical recovery.
The Role of Exercise in Constipation

The Role of Exercise in Constipation Introduction: Constipation is a common digestive issue that can lead to discomfort and frustration. While dietary adjustments and hydration play a crucial role in managing constipation, exercise is often an overlooked yet highly effective solution. In this article, we’ll explore how regular physical activity can help alleviate constipation and promote a healthy digestive system. Understanding Constipation: Before delving into the role of exercise, let’s briefly understand what constipation is. Constipation occurs when bowel movements become less frequent and stools become hard, making them difficult to pass. It can be caused by various factors, including a low-fiber diet, dehydration, lack of physical activity, and certain medical conditions. How Exercise Affects Digestion: Regular exercise stimulates the muscles in your gastrointestinal tract, which helps move waste through your intestines. This increased muscle activity, along with improved blood flow, can contribute significantly to relieving constipation. Additionally, exercise can help reduce stress levels, which can indirectly impact your digestive system. Types of Exercises Beneficial for Constipation: 1. Aerobic Activities: Engaging in aerobic exercises like walking, jogging, swimming, and cycling can help increase heart rate and improve blood circulation. This enhanced blood flow to the digestive organs can aid in more efficient bowel movements. 2. Core-Strengthening Exercises: Core exercises, such as planks, yoga, and Pilates, target the muscles in your abdomen and lower back. Strengthening these muscles can lead to improved abdominal function, which can help prevent and alleviate constipation. 3. Pelvic Floor Exercises: Kegel exercises, often associated with improving bladder control, can also benefit the muscles involved in bowel movements. These exercises can help regulate the passage of stool. 4. Stretching and Yoga: Gentle stretching exercises and yoga poses that focus on the abdomen can help relieve tension in the digestive tract. They also promote relaxation, which is essential for healthy digestion. Tips for Incorporating Exercise into Your Routine: 1. Start Slowly: If you’re new to exercise, begin with low-impact activities and gradually increase intensity and duration. 2. Consistency is Key: Aim for at least 30 minutes of moderate exercise most days of the week for optimal digestive health. 3. Stay Hydrated: Remember to drink plenty of water before, during, and after your exercise routine to prevent dehydration, which can exacerbate constipation. 4. Listen to Your Body: Pay attention to how your body responds to different exercises. If something doesn’t feel right, adjust or try a different activity. Conclusion: Regular exercise is a powerful tool in managing constipation and promoting overall digestive health. By incorporating a variety of exercises into your routine, you can help keep your gastrointestinal tract in optimal condition. Remember to consult with a healthcare professional if you have persistent or severe constipation, as it may be a sign of an underlying medical condition. With a balanced approach to diet, hydration, and exercise, you can achieve and maintain a healthy, regular digestive system. Disclaimer: Always consult with a healthcare professional before starting a new exercise program, especially if you have pre-existing medical conditions.
Effective Strategies for Piles Treatment

Introduction: Piles, also known as hemorrhoids, are a common condition that affects millions of people worldwide. Characterized by swollen and inflamed blood vessels in the rectal area, piles can cause discomfort, pain, and even bleeding. However, the good news is that there are various effective strategies available for piles treatment that can bring relief and aid in the recovery process. Understanding Piles: Before diving into the treatment options, it’s important to understand the two types of piles: internal and external. Internal piles are located inside the rectum and are usually painless but can cause bleeding. External piles, on the other hand, are located under the skin around the anus and can be quite painful. 1. Lifestyle Modifications: One of the first steps in treating piles is making necessary lifestyle changes. Maintaining a high-fiber diet is crucial to prevent constipation, a common trigger for piles. Consuming fruits, vegetables, whole grains, and drinking plenty of water can soften stools and ease bowel movements. Avoiding straining during bowel movements and establishing a regular bathroom schedule can further reduce the risk of aggravating piles. 2. Over-the-Counter Treatments: For mild cases of piles, over-the-counter creams, ointments, and suppositories can provide temporary relief from pain, itching, and inflammation. These products usually contain ingredients like witch hazel or hydrocortisone, which help shrink swollen blood vessels and reduce discomfort. 3. Sitz Baths: A sitz bath involves soaking the anal area in warm water for about 15 minutes. This can help alleviate pain, itching, and inflammation associated with piles. Adding Epsom salts to the water may provide additional relief. Sitz baths can be done a few times a day to help improve blood circulation and promote healing. 4. Medications: In some cases, a doctor may prescribe medications to manage pain, reduce inflammation, and promote healing. Non-steroidal anti-inflammatory drugs (NSAIDs) or prescription creams may be recommended to help ease symptoms. 5. Minimally Invasive Procedures: For more severe cases of piles, minimally invasive procedures may be considered. These include rubber band ligation, where a small rubber band is placed around the base of the pile to cut off its blood supply, causing it to shrink and fall off. Another option is sclerotherapy, where a chemical solution is injected into the pile to shrink it. 6. Surgical Options: Surgery is typically reserved for severe or recurrent cases of piles that do not respond to other treatments. Surgical options include hemorrhoidectomy, where the piles are surgically removed, and stapled hemorrhoidopexy, which involves stapling the piles back into place. Conclusion: Piles can be uncomfortable and even painful, but effective treatment strategies are available to provide relief and promote healing. Whether through lifestyle modifications, over-the-counter treatments, minimally invasive procedures, or surgical options, it’s important to consult a healthcare professional to determine the most suitable approach for your specific condition. Remember, early intervention and proper care can make a significant difference in managing piles and improving your overall quality of life.
