Understanding Pilonidal Sinus – Causes, Symptoms, and Treatment Options
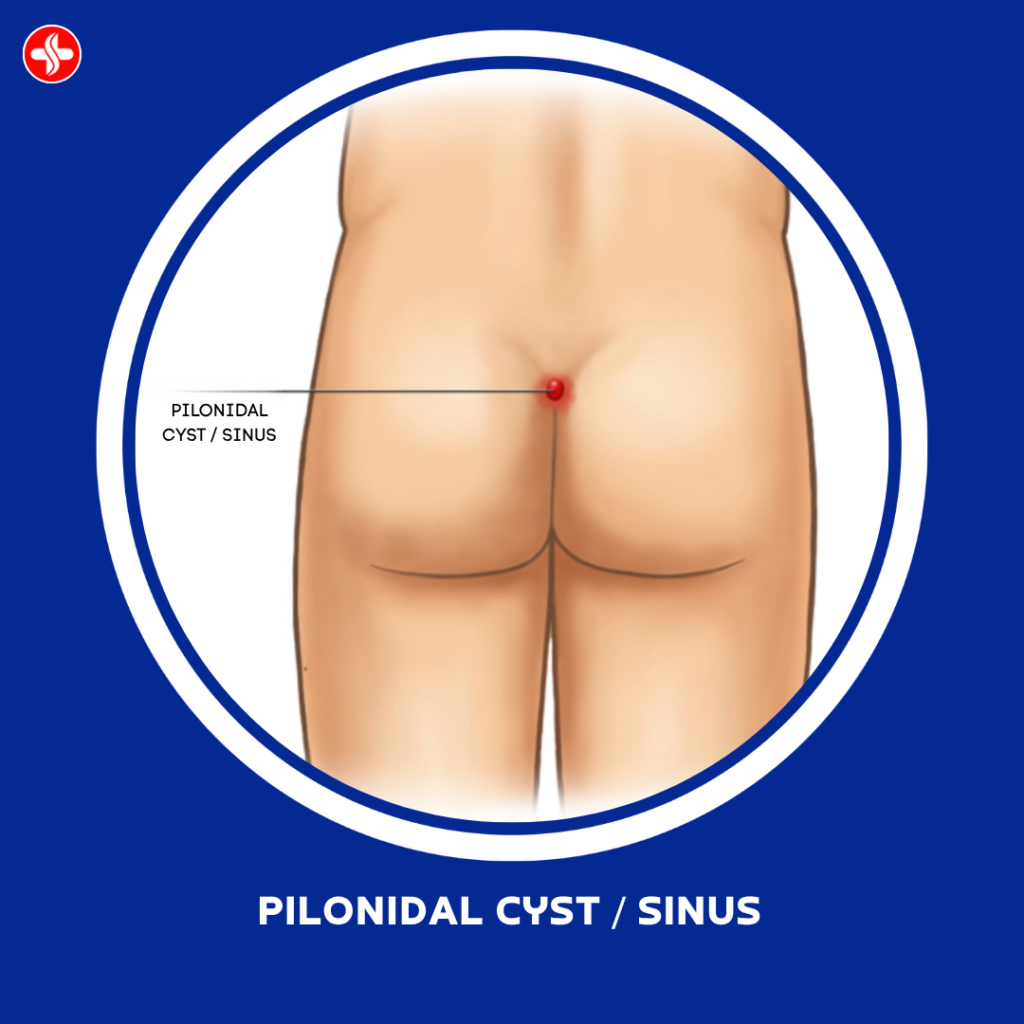
Pilonidal sinus, often called “Jeep disease” due to its historical prevalence among soldiers riding in military jeeps, is a common yet discomforting condition affecting the skin near the tailbone (coccyx). This condition typically occurs when hair follicles become embedded and cause an infection. Here’s a comprehensive look into its causes, symptoms, and advanced treatment options available at Medbros Surgery Clinic, Dehradun. Causes and Risk Factors – Pilonidal sinus develops when hair punctures the skin and becomes embedded. This can lead to inflammation and infection. Several factors contribute to its development: Hair Growth: Excessive hair growth in the buttock area can increase the risk. Friction: Constant rubbing or irritation from tight clothing or sitting for prolonged periods. Congenital Factors: Some individuals may have a predisposition due to congenital factors like the shape of the buttocks or excessive sweating. Symptoms – The symptoms of pilonidal sinus can vary depending on the severity of the condition: Pain : Persistent pain in the lower spine area. Swelling : Redness and swelling around the tailbone. Drainage : Pus or blood draining from the sinus openings. Fever : In severe cases, fever may occur due to infection. Treatment Options – Traditionally, treatment for pilonidal sinus involved surgical procedures such as excision and drainage. However, recent advancements in medical technology have introduced minimally invasive options, including hybrid laser surgery. Hybrid Laser Surgery at Medbros Surgery Clinic – Medbros Surgery Clinic, under the expert guidance of Dr. Shivam Verma, offers state-of-the-art hybrid laser surgery for pilonidal sinus. This innovative approach combines the precision of laser technology with minimally invasive techniques, ensuring: Faster Recovery : Reduced trauma to surrounding tissues leads to quicker healing times. Minimal Scarring : Laser technology enables precise incisions, minimizing visible scarring post-surgery. Reduced Risk of Recurrence : Comprehensive removal of sinus tracts reduces the likelihood of recurrence. Advantages of Hybrid Laser Surgery – Hybrid laser surgery offers several advantages over traditional methods : Precision : Laser technology allows precise targeting of infected tissues while sparing healthy ones. Patient Comfort : Minimally invasive techniques reduce discomfort during and after surgery. Outpatient Procedure : Many patients can return home the same day, promoting a faster return to daily activities. Conclusion – At Medbros Surgery Clinic, we prioritize patient comfort and clinical excellence. Dr. Shivam Verma and his team specialize in the latest advancements in surgical care, ensuring optimal outcomes for patients suffering from pilonidal sinus. If you or a loved one is experiencing symptoms of pilonidal sinus, don’t hesitate to consult with us for personalized care and treatment options.
What Are Anal Warts? Causes, Symptoms & When to See a Doctor !

Anal warts may not be a topic people feel comfortable talking about, but they are more common than most realize. These small, flesh-colored bumps around or inside the anus can start out unnoticed — but left untreated, they may grow and cause discomfort or embarrassment. In this article, we’ll break down everything you need to know about anal warts: what causes them, the symptoms to watch for, and when it’s time to see a doctor. What Are Anal Warts? Anal warts, also called condyloma acuminata, are a type of genital wart caused by certain strains of the human papillomavirus (HPV). They appear as small growths in and around the anus and can vary in size, shape, and number. Some are so tiny they go unnoticed, while others can multiply and form clusters that resemble cauliflower. They are usually benign (non-cancerous), but the condition can progress if not treated — especially if caused by high-risk strains of HPV. What Causes Anal Warts? The primary cause of anal warts is infection with HPV, especially types 6 and 11, which are considered low-risk for cancer but high-risk for wart formation. HPV is transmitted through: Unprotected anal, vaginal, or oral sex Skin-to-skin contact with an infected area Sharing of sex toys In some rare cases, even non-sexual transmission through touch It’s important to note that HPV is incredibly common — most sexually active adults will contract it at some point, often without even knowing it. Who Is at Risk? Anyone who is sexually active can develop anal warts, but certain factors increase your risk: Having multiple sexual partners Having unprotected sex Engaging in receptive anal intercourse A weakened immune system (e.g., HIV-positive individuals) History of other STIs Symptoms of Anal Warts Anal warts can vary from barely noticeable to highly irritating. Common symptoms include: Small, soft, flesh-colored bumps around the anus Itching or discomfort in the anal area Bleeding during bowel movements A sensation of a lump or fullness near the anus Mucus discharge Sometimes, anal warts can grow inside the anal canal, making them invisible externally — but they may still cause discomfort or bleeding. When to See a Doctor It’s crucial to seek medical attention if you notice: Any new growths or bumps around your anal or genital area Persistent anal itching or irritation Bleeding from the rectum without an obvious cause (like hemorrhoids) A partner is diagnosed with HPV or genital warts Early diagnosis can help prevent the spread of warts and reduce the risk of complications like recurrence or progression to pre-cancerous changes. How Are Anal Warts Treated? Treatment options depend on the size, number, and location of the warts. Common methods include: Prescription creams (e.g., imiquimod, podofilox) Cryotherapy (freezing the warts) Electrocautery (burning off warts with an electric current) Surgical excision Laser therapy (especially effective for larger or internal warts) Even after treatment, HPV can remain in the body, so recurrence is possible. Regular follow-up is often recommended. Prevention Tips While there’s no guaranteed way to avoid HPV entirely, these steps can significantly lower your risk: Get the HPV vaccine (recommended for people up to age 45) Use condoms and dental dams during sex Limit the number of sexual partners Practice good hygiene Avoid sharing sex toys or clean them thoroughly between uses Final Thoughts Anal warts can be distressing, but they are treatable and manageable with the right care. Don’t let stigma or embarrassment delay you from getting checked — early diagnosis and treatment can make a big difference in your comfort and long-term health. If you’re experiencing symptoms or simply want peace of mind, consult a qualified proctologist or sexual health expert today.
The Importance of MRI Fistulogram Before Anal Fistula Surgery

Anal fistulas can be complex and challenging conditions to treat effectively. Before undergoing surgery for an anal fistula, it is crucial to assess the anatomy and extent of the fistula tract accurately. One of the most effective diagnostic tools in this regard is the MRI fistulogram. Here’s why it’s essential: 1. Accurate Assessment of Fistula Anatomy: MRI fistulogram provides detailed imaging of the fistula tract, including its path, branches, and relation to surrounding structures. This information is critical for surgical planning as it helps the surgeon understand the complexity of the fistula and decide the best approach for treatment. 2. Identification of Secondary Tracts and Extensions: Anal fistulas can have secondary tracts or extensions that may not be visible externally. MRI fistulogram can detect these hidden tracts, which are crucial to address during surgery to prevent recurrence. 3. Evaluation of Adjacent Structures: The MRI fistulogram also evaluates nearby structures such as the anal sphincters and pelvic floor muscles. This assessment is vital as preserving sphincter function is a primary goal of fistula surgery. 4. Guidance for Surgical Planning: Armed with detailed MRI fistulogram images, surgeons can create a precise surgical plan tailored to each patient’s specific anatomy. This personalized approach improves surgical outcomes and reduces the risk of complications. 5. Prevention of Recurrence: By accurately mapping the fistula tract and its extensions, MRI fistulogram helps ensure thorough removal during surgery. This reduces the likelihood of recurrence, which is a common challenge in fistula management. 6. Patient Comfort and Safety: Unlike traditional methods such as probing or examination under anesthesia, MRI fistulogram is non-invasive and does not require the patient to be under anesthesia. This enhances patient comfort and safety during the diagnostic process. Conclusion: MRI fistulogram plays a crucial role in the management of anal fistulas by providing comprehensive anatomical information that guides surgical decision-making and improves treatment outcomes. Before undergoing anal fistula surgery, consulting with a specialist who utilizes MRI fistulogram can significantly enhance the quality and success of the surgical intervention. Understanding the importance of MRI fistulogram in anal fistula surgery empowers patients and healthcare providers to make informed decisions that prioritize long-term health and well-being.
Best Piles Doctor in Dehradun, Uttarakhand !
🩺 Best Piles, Fissure, Fistula Doctor in Dehradun, Uttarakhand – Dr. Shivam Verma (M.S, F.ICRS, F.MAS, D.MAS, F.GIE) Consultant Proctologist & GI Endoscopist (Laser, Laparoscopic & Robotic Surgeon) Are you suffering from piles, anal fissure, or fistula and searching for the best specialist in Dehradun or Uttarakhand ? Your search ends here. Meet Dr. Shivam Verma — India’s First Ayurvedic Qualified Robotic Surgeon and Certified Hybrid Laser Proctologist. With 9+ years of surgical experience and thousands of successful procedures, Dr. Verma is one of the most trusted and advanced proctology experts in North India. 🌟 Why Dr. Shivam Verma Is the #1 Choice for Piles, Fissure & Fistula in Dehradun: ✅ Certified Hybrid Laser Proctologist of Neo-V Laser (Israel)✅ Fellowship in International College of Robotic Surgeons (F.ICRS)✅ Fellowship & Diploma in Minimal Access Surgery (F.MAS, D.MAS)✅ Fellowship in Gastrointestinal Endoscopy (F.GIE)✅ Member, National Sushruta Association (NSA), WALS, EAES, SAGES✅ Registered with National Commission for Indian System of Medicine (NCISM)✅ Certified Surgeon under National Health Authority (Govt. of India) Member – NSA, NCISM, WALS, SAGES, EAES, NHA 📍 Practicing at Medbros Surgery Clinic, Dehradun – A Leading Center for Hybrid Laser and Robotic Surgery ! Medbrosurgery.com is Dehradun’s most advanced, transparent surgical platform, offering 100% evidence-based care in Proctology. Hybrid Proctology is an advanced, integrated approach that combines the precision of modern laser surgery with the holistic healing principles of Ayurveda and evidence-based minimally invasive techniques. It is especially effective for complex and chronic anorectal conditions like: Piles (Hemorrhoids). Anal Fissure. Complex Fistula-in-Ano. Pilonidal Sinus. Perianal Abscesses. Sentinel Tags & Rectal Polyps. ✨ What Makes Dr. Shivam Verma’s Hybrid Approach Unique? ✅ Laser + Ayurvedic Therapy: Combines laser ablation with customized Ayurvedic formulations and Kshar Sutra (where applicable) to minimize recurrence and promote faster healing. ✅ Minimal Access & Robotic Precision: Uses advanced endoscopic and robotic-assisted tools (where indicated) for accurate tissue targeting with zero collateral damage. ✅ Day-Care, Painless Procedures: Performed under local or spinal anesthesia, these surgeries allow same-day discharge with minimal discomfort. ✅ Holistic Recovery Protocol: Post-operative care includes diet, lifestyle advice, pain management, Ayurvedic wound healing support, and regular follow-ups for sustained relief. 🧬 Benefits of Hybrid Proctology at Medbros Surgery Clinic : ✔️ Painless Laser Treatment✔️ Faster Wound Healing & Recovery✔️ Minimal Bleeding & No Stitches✔️ Reduced Hospital Stay (Daycare)✔️ Lower Risk of Recurrence✔️ Evidence-Based + Ayurveda-Informed Protocols — 💬 Patient Reviews & Testimonials : On May 22/2025 i visited Medbros clinic for my constipation and intestinal crampring issue , which i have been suffering from last 1 and a half year , i booked an appointment with Dr. Shivam , i told him my problem to which he acknowledged every single issue very paciently and attentively he is very polite and humble one of the finest doctor in my experience so far. I am surprised my stomach cramping got resolved in the very first dose of his prescribed medicine and i am relieved from intestinal ache with in 24 hrs Thank you Dr shivam 🙏🏻 Major recommendation for all those who has been suffering from any kind of stomach disease you must go and consult Dr. Shivam. – Mr. Shubham Sharma (Dehradun) 2. डॉ. शिवम् वर्मा पाइल्स के उपचार के क्षेत्र में बहुत अच्छा अनुभव और विशेषज्ञता रखते हैं। उनका नर्सिंग स्टाफ भी बहुत प्रोफेशनल और मृदु व्यवहार वाले हैं। उन्होंने मेरा पाइल्स का ऑप्रेशन कर मात्र 10 दिनों में स्वस्थ कर दिया हैं। डॉ. शिवम् वर्मा और उनकी टीम को मेरा धन्यवाद. बलबीर सिंह, कोटद्वार, उत्तराखंड। -Mr. Balbir Singh (Kotdwar) 3.”I had problems with chronic fissure and hemorrhoids. Through a Google search, I came to know about Dr. Shivam Verma. At that time, I was struggling with severe pain and was not even in a condition to speak properly. However, Sir understood my pain very well, carefully diagnosed me, and started the treatment. Because of me, Sir and his staff often stayed late at night, and this happened many times later as well. Yet, they always handled me respectfully and patiently. Sir truly gives the highest value to his patients. Talking about the surgery, Dr. Shivam Verma and his team were like magicians for me because I did not face any kind of difficulty. There were a few sessions of mild pain, but with Sir’s experience and excellent treatment, everything healed completely. Illness not only weakens you physically but also mentally, and Dr. Shivam Verma helped me come out of it. No matter how much I thank him, it will never be enough. I wholeheartedly send him lots of blessings. Thank you so much Sir.” -Mrs. Anjana Ravi (Haridwar) 4.I was very upset for 6-7 years due to fistula disease and I also consulted many doctors. But I was not given the need to recover completely by any doctor. All of them mentioned the repetition. Then I came to know about Dr. Shivam Verma Sir and I met him and told my problem. Then he requested me that this problem will not repeat. He is one of the best doctors. Doctor Shivam Sir treats the patient like family members. Once he started my treatment, I was mentally relieved. Just I do not have the appropriate word to praise Dr. Shivam Sir and all the staff of the hospital are very good. I am writing a review after 3 months today and Dr. Shivam Sir told me till the last that I am completely fine. Thank you to Dr. Shivam Sir with heart for freeing me from fistula.I want to speak to all the patients who suffer from these diseases. He must consult Dr. Shivam sir once. -Mr. Rajesh Tiwari (Haridwar) 5. Dr. Shivam Verma is expertise in his field highly educated, very attentive. Medical coordinator took great care of my treatment. Staff was very cooperative. 100% recommended. -Ms. Anita Birla (Dehradun) 📈 Google Rankings & Reputation : Dr. Shivam Verma consistently ranks among the Top 3 Proctology & Laser Surgery Doctors on : Google Local Search (Maps) JustDial & Practo National Digital Health
Understanding Bleeding and Mucus Discharge After Piles and Fissure Surgery

Are you a patient who has recently undergone piles or anal fissure surgery ? If you are experiencing bleeding and mucus discharge after the procedure, you might be worried about what these symptoms. In this blog post, we will delve into the about bleeding and mucus discharge post-surgery to provide you with valuable insights and peace of mind. What Causes Bleeding After Piles and Fissure Surgery? Bleeding after piles or fissure surgery is a common concern for many patients. It is essential to understand that a small amount of bleeding can be normal post-surgery as the body heals. The following factors may contribute to bleeding after the procedure: Residual Tissue: Sometimes, small amounts of residual tissue can lead to bleeding after surgery. This is a natural part of the healing process, and the bleeding should subside as your body continues to heal. Dietary Changes: Changes in your diet post-surgery, such as an increase in fiber intake, can also cause minor bleeding as your digestive system adjusts. Straining: Straining during bowel movements can put pressure on the healing tissues, leading to minor bleeding. It is crucial to avoid straining and follow your healthcare provider’s instructions for a smooth recovery. Understanding Mucus Discharge Post-Surgery Apart from bleeding, many patients may also experience mucus discharge after piles or fissure surgery. While this symptom can be disconcerting, it is essential to recognize that mucus discharge is a normal part of the healing process. Here are some reasons why mucus discharge may occur post-surgery: Inflammation: The surgical site may produce mucus as a natural response to inflammation. This mucus helps protect the area and aids in the healing process. Wound Healing: Mucus discharge can be a sign that the wound is healing correctly, and the body is working to remove any debris or infection from the area. Coping Strategies for Bleeding and Mucus Discharge If you are experiencing bleeding or mucus discharge after piles or fissure surgery, there are several coping strategies you can implement to manage these symptoms effectively: Follow Your Doctor’s Advice: It is crucial to follow your healthcare provider’s instructions regarding wound care, diet, and activity restrictions post-surgery. Stay Hydrated: Drinking plenty of water can help soften your stool and ease bowel movements, reducing the risk of straining and bleeding. Maintain Good Hygiene: Proper hygiene is essential to prevent infection and promote healing. Keep the surgical site clean and dry to minimize the risk of complications. Remember, it is normal to experience some bleeding and mucus discharge after piles or fissure surgery. However, if you have concerns or persistent symptoms, do not hesitate to seek medical advice promptly. A Final Thought In conclusion, bleeding and mucus discharge after piles and fissure surgery are common occurrences during the recovery process. By understanding the reasons behind these symptoms and implementing proper coping strategies, you can navigate through this phase with confidence and peace of mind. Remember to be patient with your body as it heals and reach out to your healthcare provider if you have any concerns. Stay informed, stay positive, and prioritize your health above all else.
How Piles Surgery Is Done

Introduction: Dealing with piles, also known as hemorrhoids, can be a challenging and uncomfortable experience. When conservative treatments fail to provide relief, piles surgery becomes a viable option. In this blog post, we’ll delve into the details of how piles surgery is performed, shedding light on the procedures involved and the recovery process. Types of Piles Surgery: There are various surgical procedures available for treating piles, and the choice depends on the severity and type of hemorrhoids. The two most common types of piles surgery are: Hemorrhoidectomy: This is a traditional surgical approach involving the removal of swollen hemorrhoidal tissue. The patient is usually placed under general anesthesia to ensure comfort during the procedure. The surgeon makes incisions around the hemorrhoids and removes the excess tissue. Sutures or surgical staples may be used to close the incisions, promoting healing. Minimally Invasive Procedures: These procedures include techniques like rubber band ligation, sclerotherapy, and laser coagulation. Rubber band ligation involves placing a rubber band around the base of the hemorrhoid to cut off its blood supply, causing it to shrink and fall off. Sclerotherapy involves injecting a solution into the hemorrhoid, leading to its shrinkage over time. Laser coagulation employs laser energy to vaporize or shrink the hemorrhoidal tissue. The Surgical Process: Preparation: Before the surgery, the patient undergoes a thorough examination and may be required to follow certain dietary and lifestyle modifications. Bowel preparation might be necessary, involving laxatives or enemas to ensure a clean and clear surgical field. Anesthesia: The choice of anesthesia depends on the type of surgery. General anesthesia is common for hemorrhoidectomy, while minimally invasive procedures may require local or regional anesthesia. Incision or Treatment Application: In hemorrhoidectomy, incisions are made around the hemorrhoidal tissue for removal. For minimally invasive procedures, the specific technique is applied. Closure: For traditional hemorrhoidectomy, the incisions are closed using sutures or staples. Minimally invasive procedures often don’t require closure. Recovery: Postoperative Care: Patients are typically monitored in a recovery area before being discharged. Pain management and stool softeners are prescribed to alleviate discomfort and prevent straining during bowel movements. Diet and Lifestyle Changes: Patients are advised to follow a high-fiber diet and stay hydrated to promote smooth bowel movements. Avoiding prolonged sitting and engaging in light physical activity can aid in the recovery process. Follow-up: Scheduled follow-up appointments are crucial to monitor the healing process and address any concerns. Conclusion: Piles surgery is a viable solution for those experiencing severe or persistent hemorrhoids. The choice of procedure depends on the individual case, and consultation with a healthcare professional is crucial. While recovery may take time, proper postoperative care and adherence to medical advice can contribute to a successful outcome. Always consult with a healthcare professional to determine the most appropriate treatment for your specific condition.
Inguinal Hernia: Causes, Symptoms, and Treatment Options

Introduction: Inguinal hernia are a common medical condition that affects a significant number of people worldwide. While not always life-threatening, they can cause discomfort and require medical attention. In this blog post, we’ll delve into the details of inguinal hernia, exploring their causes, symptoms, and available treatment options. What is an Inguinal Hernia? An inguinal hernia occurs when a portion of the intestine or other abdominal tissue protrudes through a weakened area or opening in the abdominal muscles, creating a bulge. This type of hernia typically occurs in the inguinal canal, a passageway in the lower abdomen near the groin. Causes: Weakness in the Abdominal Wall: In many cases, inguinal hernias develop due to a weakness in the abdominal muscles, which may be present from birth or develop over time. Increased Intra-Abdominal Pressure: Conditions that increase pressure within the abdomen, such as heavy lifting, chronic coughing, or obesity, can contribute to the development of an inguinal hernia. Age and Gender: Men are more prone to inguinal hernias than women, and the risk tends to increase with age. Symptoms: Visible Bulge: The most common and noticeable symptom of an inguinal hernia is a bulge in the groin area. This bulge may become more prominent when standing, coughing, or straining. Pain or Discomfort: Discomfort or pain in the groin, especially when lifting heavy objects or during physical activity, may accompany an inguinal hernia. Aching or Burning Sensation: Some individuals with inguinal hernias report aching or burning sensations around the bulge. Pressure in the Abdomen: Patients may experience a feeling of pressure or heaviness in the abdomen. Treatment Options: Watchful Waiting: In some cases, especially when the hernia is small and not causing significant discomfort, a “watchful waiting” approach may be recommended. Regular monitoring and lifestyle adjustments may be suggested. Hernia Truss: A hernia truss is a supportive device that can be worn to help keep the hernia in place. While it can provide relief, it is not a long-term solution and is generally used in cases where surgery is not immediately possible. Surgery: The most common and effective treatment for inguinal hernias is surgery. During the procedure, the protruding tissue is pushed back into place, and the weakened abdominal wall is repaired. With advancements in surgical techniques, many inguinal hernia repairs are now done using minimally invasive laparoscopic methods. Conclusion: Understanding the causes, symptoms, and treatment options for inguinal hernias is crucial for early detection and appropriate management. If you suspect you have an inguinal hernia or are experiencing related symptoms, it is essential to consult with a healthcare professional for a thorough evaluation and personalized treatment plan. Early intervention can help alleviate discomfort and prevent complications associated with inguinal hernia.
Preventing Kidney Stones Recurrence

A Comprehensive Guide to Preventing Kidney Stones Recurrence Introduction: Kidney stones, though small, can wreak havoc on one’s well-being. Anyone who has experienced the excruciating pain and discomfort of kidney stones is well aware of the importance of preventing their recurrence. In this comprehensive guide, we will explore effective strategies and lifestyle changes to defy the odds and keep kidney stones at bay. Understanding the Enemy: Before we delve into prevention strategies, it’s crucial to understand what causes kidney stones. These hard deposits form when certain substances in the urine — such as calcium, oxalate, and phosphorus — become highly concentrated. By comprehending the enemy, we can better strategize to prevent its return. Hydration: The Ultimate Weapon: One of the simplest yet most powerful weapons against kidney stones is staying well-hydrated. Drinking an ample amount of water dilutes the substances in the urine that lead to stones. Aim for at least 8 cups of water a day, and increase intake during hot weather or periods of intense physical activity. Dietary Changes for Stone Prevention: Mindful Calcium Consumption: Contrary to popular belief, adequate calcium intake can reduce the risk of kidney stones. Choose calcium-rich foods over supplements and ensure a balanced diet. Moderating Oxalate Intake: Oxalate is found in certain foods, and high consumption can contribute to stone formation. Limiting the intake of oxalate-rich foods such as spinach, beets, and nuts can be beneficial. Sodium Reduction: High sodium intake can increase calcium levels in the urine, promoting stone formation. Opt for fresh, whole foods and limit processed and packaged items. Watch the Protein: Diets high in animal proteins may lead to higher levels of uric acid and calcium in the urine. Consider incorporating plant-based protein sources and moderating meat consumption. Lifestyle Modifications: Regular Exercise: Physical activity promotes overall health and can aid in preventing obesity, a risk factor for kidney stones. Aim for at least 150 minutes of moderate-intensity exercise per week. Maintain a Healthy Weight: Obesity is linked to an increased risk of kidney stones. Adopting a healthy, balanced diet and regular exercise can help maintain an optimal weight. Limit Caffeine and Alcohol: Excessive caffeine and alcohol consumption can contribute to dehydration. Moderation is key, and balancing these beverages with water intake is advisable. Medical Interventions and Follow-Up: Medication Compliance: For individuals with a history of certain types of stones, medications may be prescribed to prevent recurrence. Adhering to the prescribed medication regimen is essential. Regular Check-ups and Monitoring: Routine follow-up with healthcare providers is crucial for monitoring urine composition and overall kidney health. Regular check-ups allow for timely intervention and adjustments to prevention strategies. Conclusion: Preventing kidney stones recurrence requires a holistic approach encompassing hydration, dietary modifications, lifestyle changes, and, in some cases, medical interventions. By adopting these strategies and maintaining a proactive stance, individuals can defy the odds and enjoy a life free from the pain and inconvenience of kidney stones. Remember, knowledge and commitment are the keys to triumph over this common yet preventable condition.
Understanding Liver Abscess

Introduction: Liver abscess is a serious medical condition that can have significant implications for an individual’s health. In this blog post, we will delve into the causes, symptoms, and treatment options for liver abscess, shedding light on this potentially life-threatening condition. What is a Liver Abscess ? A liver abscess is a pus-filled cavity within the liver that can develop due to various infections. It is a relatively rare condition but requires prompt medical attention when diagnosed. The two main types of liver abscess are: Pyogenic Liver Abscess: This type is typically caused by bacterial infections, with the bacteria often reaching the liver through the bloodstream or from an infection in the abdominal area. Amoebic Liver Abscess: Amoebic liver abscess is caused by the parasite Entamoeba histolytica. This type is more common in regions with poor sanitation and hygiene. Causes of Liver Abscess: Pyogenic Liver Abscess: Bacterial infection in the abdomen, such as appendicitis or diverticulitis. Infection spreading through the bloodstream from other parts of the body. Recent abdominal surgery. Biliary tract infections. Amoebic Liver Abscess: Ingestion of contaminated food or water. Poor sanitation and hygiene practices. Symptoms of Liver Abscess: Abdominal Pain: Pain in the upper right side of the abdomen is a common symptom. Fever and Chills: Patients may experience fever and chills as the body responds to the infection. Jaundice: Yellowing of the skin and eyes due to impaired liver function. Unexplained Weight Loss: Rapid weight loss without apparent cause. Nausea and Vomiting: Feeling nauseous and vomiting may occur. Changes in Stool Color: Dark-colored urine and light-colored stools may be observed. Diagnosis and Treatment: Diagnostic Tests: Blood tests, including liver function tests. Imaging studies such as ultrasound, CT scans, or MRI to visualize the liver. Aspiration of the abscess for laboratory analysis. Medical Treatment: Antibiotics are prescribed to treat bacterial infections. Antiparasitic medications for amoebic liver abscess. Pain management medications. Drainage Procedures: Large abscesses may require drainage to remove pus and reduce pressure on the liver. Drainage may be done through needle aspiration or catheter placement. Hospitalization: Severe cases or complications may require hospitalization for close monitoring and intravenous treatment. Prevention: Hygiene Practices: Practice good hygiene, especially handwashing, to prevent amoebic infections. Prompt Treatment of Infections: Timely treatment of infections in the abdominal region to prevent the spread to the liver. Vaccination: In some cases, vaccination against certain infections may be recommended. Conclusion: Liver abscess is a serious condition that demands swift medical intervention. Recognizing the symptoms, understanding the causes, and seeking prompt medical attention can significantly improve the prognosis. As with many health conditions, prevention through good hygiene practices and addressing infections promptly is key. If you suspect you or someone you know may have a liver abscess, consult a healthcare professional for a comprehensive evaluation and appropriate treatment.
Pediatric General Surgery

Introduction: When it comes to the health and well-being of our little ones, parents understandably seek the best care available. Pediatric general surgery is a specialized field dedicated to addressing surgical concerns unique to children. In this blog post, we’ll explore the special considerations and procedures involved in pediatric general surgery, shedding light on the intricacies of caring for our youngest patients. 1. Specialized Expertise: The Pediatric Surgeon’s Role Pediatric surgeons are medical professionals with specialized training in performing surgeries on infants, children, and adolescents. Their expertise goes beyond surgical skills; they understand the nuances of pediatric anatomy, growth patterns, and the emotional needs of young patients and their families. 2. Common Conditions Requiring Pediatric Surgery: Hernias: While hernias can occur at any age, they are relatively common in infants and children. Pediatric surgeons use minimally invasive techniques to repair hernias with a focus on gentle, effective care. Appendicitis: Appendicitis can affect children as well, often requiring prompt surgical intervention. Pediatric surgeons are adept at diagnosing and addressing this condition while considering the unique aspects of a child’s physiology. Congenital Anomalies: Some children are born with structural abnormalities that may require surgical correction. Pediatric general surgeons collaborate with other specialists to address conditions such as congenital heart defects, intestinal malformations, and more. 3. Minimally Invasive Approaches: Advancements in medical technology have paved the way for minimally invasive surgery in pediatric patients. Techniques such as laparoscopy and robotic-assisted surgery offer smaller incisions, reduced postoperative pain, and faster recovery times. Pediatric general surgeons leverage these innovations to ensure the best outcomes for their young patients. 4. Anesthesia Considerations: Administering anesthesia to children requires a delicate balance. Pediatric anesthesiologists work closely with general surgeons to tailor anesthesia plans based on a child’s age, weight, and overall health. The goal is to ensure a safe and comfortable experience for the child during surgery. 5. Family-Centered Care: Pediatric general surgery extends beyond the operating room. These surgeons recognize the importance of family-centered care, involving parents and caregivers in the decision-making process and providing support throughout the entire surgical journey. 6. Emotional Well-being of Pediatric Patients: Children may experience anxiety or fear before surgery. Pediatric general surgeons and healthcare teams take extra steps to create a child-friendly environment, explain procedures in age-appropriate language, and use play therapy to alleviate anxiety and build trust. 7. Postoperative Care and Follow-up: Recovery is a crucial phase, and pediatric general surgeons work closely with postoperative care teams to monitor a child’s progress. Clear communication with parents is maintained to ensure proper at-home care and address any concerns promptly. Conclusion: Pediatric general surgery is a specialized field that combines surgical expertise with a deep understanding of pediatric medicine and the unique needs of children. From common conditions to congenital anomalies, the focus is on providing effective, compassionate care tailored to the developmental stage of each young patient. Parents can rest assured that when it comes to the surgical well-being of their children, pediatric general surgeons are dedicated to navigating the path to recovery with expertise, empathy, and a commitment to the health and happiness of the littlest members of our families.
